Dialectical Behavioural Therapy (DBT)
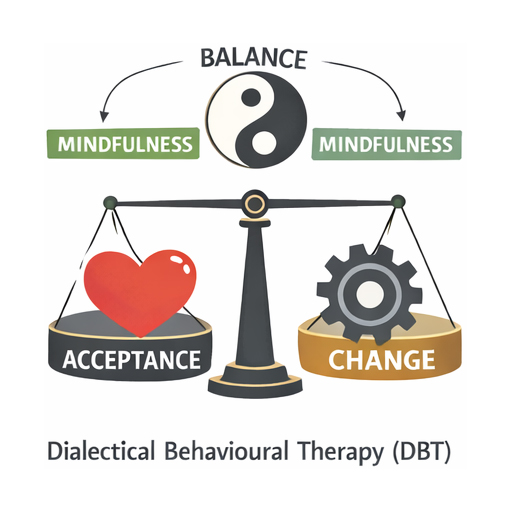
DBT combines cognitive-behavioural strategies with mindfulness. It teaches skills in four areas including Distress Tolerance, Emotion Regulation, Interpersonal Effectiveness and Mindfulness.
What is DBT?
Dialectical Behaviour Therapy (DBT) is an evidence-based form of psychotherapy developed by psychologist Marsha Linehan in the late 1980s. Originally designed for individuals with borderline personality disorder (BPD), DBT has since been adapted to treat a range of mental health conditions, including depression, anxiety, eating disorders, and substance use disorders.
DBT combines cognitive-behavioural techniques with mindfulness practices, emphasising a balance between acceptance and change. This approach helps individuals manage intense emotions, reduce self-destructive behaviours, and improve interpersonal relationships.
The therapy focuses on four core skill areas: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. Delivered through individual sessions, group skills training, and phone coaching, DBT equips clients with practical tools to build a life worth living while fostering resilience and emotional stability.
- Emotional dysregulation
- Impulsivity
- Self-harm behaviours
- Suicidal thoughts or behaviours
- Chronic feelings of emptiness
- Intense anger or mood swings
- Interpersonal conflict and instability
- Difficulty tolerating distress
What are the underlying scientific principles?
Dialectical Behavioural Therapy (DBT) is a psychological treatment rooted in cognitive-behavioural principles, enriched by mindfulness and acceptance strategies. Developed by Marsha Linehan, DBT aims to help individuals regulate emotions, tolerate distress, and improve interpersonal effectiveness. It integrates behavioural science with dialectical philosophy, emphasising balance between acceptance and change. DBT is widely used for borderline personality disorder, emotional dysregulation, and self-destructive behaviours. Its scientific foundation lies in behavioural psychology, mindfulness practices from Eastern traditions, and dialectical thinking, which promotes synthesis of opposing ideas. This evidence-based approach combines structured skills training with therapeutic validation to foster resilience and adaptive coping.
Behavioural Psychology
Cognitive Restructuring
Dialectical Philosophy
Mindfulness-Based Principles
Borrowing from Zen and neuroscience, DBT incorporates mindfulness to enhance present-moment awareness. This reduces automatic reactions, improves emotional clarity, and strengthens attention regulation through evidence-based meditative practices.
Emotion Regulation Science
DBT targets biological and psychological mechanisms of emotional dysregulation. It teaches skills to modulate intensity, duration, and expression of emotions, reducing impulsivity and promoting adaptive responses under stress.
Interpersonal Effectiveness
Rooted in social psychology, DBT emphasises assertiveness and relational balance. Skills training improves communication, boundary-setting, and conflict resolution, fostering healthier relationships and reducing interpersonal chaos.
How does it work?
Dialectical Behavioural Therapy (DBT) is a structured, evidence-based approach designed to help individuals manage intense emotions and improve interpersonal relationships. Originally developed for borderline personality disorder, DBT combines cognitive-behavioural techniques with mindfulness practices. It focuses on balancing acceptance and change, empowering individuals to regulate emotions, tolerate distress, and communicate effectively. DBT is widely used for conditions involving emotional dysregulation, such as anxiety, depression, and self-harm behaviours. Through individual therapy, group skills training, and phone coaching, DBT equips clients with practical tools to navigate life’s challenges while fostering resilience and self-awareness.
Core Philosophy
DBT integrates acceptance and change strategies, teaching clients to acknowledge emotions while actively working towards behavioural adjustments, creating balance between self-acceptance and personal growth.
Skills Modules
Four modules—mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness—provide practical tools for managing emotions, reducing impulsivity, and improving relationships.
Mindfulness Practice
Mindfulness is central to DBT, helping individuals stay present, observe thoughts without judgement, and respond thoughtfully rather than react impulsively to emotional triggers.
Distress Tolerance
This module teaches coping strategies for crises, such as distraction, self-soothing, and radical acceptance, enabling individuals to endure emotional pain without harmful behaviours.
Emotion Regulation
Clients learn to identify, understand, and modify emotional responses, reducing vulnerability to intense feelings and promoting stability through healthy habits and coping mechanisms.
Interpersonal Effectiveness
Focuses on assertive communication, setting boundaries, and maintaining relationships while respecting personal needs, reducing conflict and fostering mutual understanding.
When Is It Used?
Dialectical Behavioural Therapy (DBT) is primarily used when individuals struggle with intense emotions that lead to harmful behaviours or interpersonal difficulties. Originally developed for borderline personality disorder, DBT is now applied to conditions such as chronic self-harm, suicidal ideation, eating disorders, and substance misuse. It is particularly effective when emotional regulation, distress tolerance, and interpersonal skills need improvement. DBT combines cognitive-behavioural techniques with mindfulness practices, helping clients build coping strategies and resilience. This structured, evidence-based approach is often chosen when traditional therapies have not been sufficient, offering practical tools for managing overwhelming feelings and fostering long-term behavioural change.
Conditions and Issues Where ACT Is Commonly Applied
Less Common or Indirect Use
What are the therapy options that Transformations Clinical Psychology can offer me?
Please contact us or follow this link if you would like to set up an assessment with a psychologist at Transformations Clinical Psychologist.
Meet Our Team
Meet our friendly and experienced team, here to help you with confidence and care.








Amy Wang
Mandarin
English


We are here to support you
Please contact us or click on this link if you would like to see one of our experienced psychologists
FAQ
Q1. What happens in the first session? Do I need to prepare?
Your first appointment is 50–60 minutes. We’ll get to know you—what’s been hard, what you’d like to change, and what’s helped before. You’re welcome to bring notes or just come as you are; we’ll go at your pace. Please complete the online intake and consent forms beforehand. Sessions are available in person (Sydney) or via secure telehealth across Australia. We’ll finish with a clear plan and time for your questions. If you’re in immediate danger, call 000.
Q2. How do fees and Medicare/private insurance work? Do I need a GP referral?
You can book without a referral. If your GP provides a Mental Health Treatment Plan, you may be eligible for a Medicare rebate. We’ll check your eligibility and confirm your out-of-pocket cost before you commit. Private health (Extras) can’t be claimed with Medicare for the same session—please check your fund for coverage. If cost is a concern, let us know and we’ll talk through options.
Q3. Will my information be kept confidential?
Yes. Your sessions and records are kept private under strict legal and ethical standards. There are a few exceptions—if there’s a serious risk of harm, concerns about a child or vulnerable person, or a court order. If we ever need to share information, we’ll explain why, what will be shared, and involve you as much as possible.
