Cognitive Behavioural Therapy (CBT)
Cognitive behavioural therapy (CBT) is a widely used intervention that is effective in treating a variety of mental health conditions. It fosters the idea that psychological problems tend to be based, in part, on unhelpful or ways of thinking and/or on learned patterns of unhelpful behaviour. Additionally, CBT emphasises that those who are dealing with psychological issues, can learn more adaptive ways of coping with them which in turn, can relieve their symptoms and improve their daily functioning.
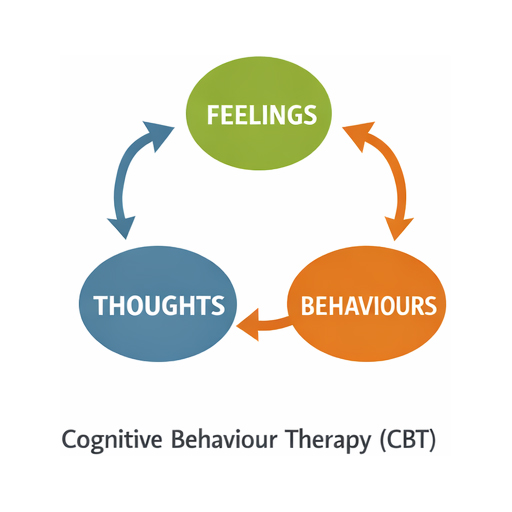
What is CBT?
Cognitive behavioural therapy (CBT) is a widely used intervention that is effective in treating a variety of mental health conditions. It fosters the idea that psychological problems tend to be based, in part, on unhelpful or ways of thinking and/or on learned patterns of unhelpful behaviour. Additionally, CBT emphasises that those who are dealing with psychological issues, can learn more adaptive ways of coping with them which in turn, can relieve their symptoms and improve their daily functioning.
What are the underlying scientific principles?
Scientific research has demonstrated that CBT can lead to significant improvements in functioning and overall quality of life. Further studies have provided evidence that CBT can be as effective as, or more effective than, other forms of psychological therapy or psychiatric medications.
How does it work?
Within the course of CBT treatment, clients are encouraged to try and change their thinking patterns. Ways in which this can be achieved include:
- Recognising that one’s distortions in thinking may be creating problems, and therefore, reevaluating their thoughts in light of reality, may be more effective.
- Gaining a more appropriate understanding of the behaviour and motivation of other people.
- Using a problem-solving approach in order to cope with difficult situations that may arise.
In conjunction with improving thoughts, CBT treatment also usually involves efforts to change one’s maladaptive behavioural patterns. These strategies might include:
- Reducing avoidance and instead, facing one’s fears.
- Engaging in role playing, between therapist and client, to prepare for the possibility of encountering problematic interactions with other people.
- Learning to engage in mindfulness to therefore, calm one’s mind and body.
What to Expect
The psychologist and client will collaboratively develop an understanding of the presenting problem and therefore, develop a treatment strategy together.
CBT places an emphasis on assisting clients to learn to be their own therapists. The client is encouraged to engage in exercises throughout the session and in the outside environment (i.e., homework), in order for clients to learn how to change their own thinking, behaviours and emotions and thus, effectively cope with any problematic situation they may encounter.
The focus of CBT is primarily on the present and moving forward in time, in order for clients to develop more effective ways of coping with life.
When is it used?
Some examples of when CBT might be used include:
- Depression
- Anxiety
- Insomnia
- Chronic pain
- Obsessive Compulsive Disorder (OCD)
- Post Traumatic Stress Disorder (PTSD)
- Substance use disorders
- Stress
What are the therapy options that Transformations Clinical Psychology can offer me?
Please contact us or follow this link if you would like to set up an assessment with a Psychologist at Transformations Clinical Psychology.
Meet Our Team
Meet our friendly and experienced team, here to help you with confidence and care.








Amy Wang
Mandarin
English


We are here to support you
Please contact us or click on this link if you would like to see one of our experienced psychologists
FAQ
Q1. What happens in the first session? Do I need to prepare?
Your first appointment is 50–60 minutes. We’ll get to know you—what’s been hard, what you’d like to change, and what’s helped before. You’re welcome to bring notes or just come as you are; we’ll go at your pace. Please complete the online intake and consent forms beforehand. Sessions are available in person (Sydney) or via secure telehealth across Australia. We’ll finish with a clear plan and time for your questions. If you’re in immediate danger, call 000.
Q2. How do fees and Medicare/private insurance work? Do I need a GP referral?
You can book without a referral. If your GP provides a Mental Health Treatment Plan, you may be eligible for a Medicare rebate. We’ll check your eligibility and confirm your out-of-pocket cost before you commit. Private health (Extras) can’t be claimed with Medicare for the same session—please check your fund for coverage. If cost is a concern, let us know and we’ll talk through options.
Q3. Will my information be kept confidential?
Yes. Your sessions and records are kept private under strict legal and ethical standards. There are a few exceptions—if there’s a serious risk of harm, concerns about a child or vulnerable person, or a court order. If we ever need to share information, we’ll explain why, what will be shared, and involve you as much as possible.
