Cognitive Behavioural Therapy (CBT)
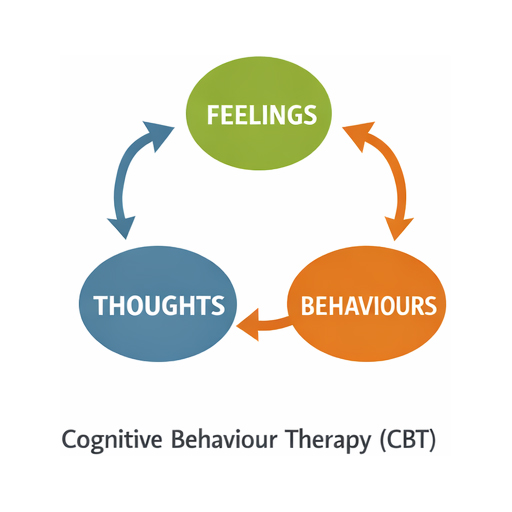
CBT focuses on identifying and challenging negative thought patterns that influence emotions and behaviours. By restructuring thoughts, individuals can change emotional responses and adopt healthier behaviours. It uses techniques like cognitive restructuring and behavioural activation.
What is CBT?
Cognitive Behavioural Therapy (CBT) is a widely used psychological treatment that focuses on the relationship between thoughts, feelings, and behaviours. It is based on the idea that negative thinking patterns can influence emotions and actions, often leading to distress.
CBT helps individuals identify and challenge these unhelpful thoughts, replacing them with more balanced and constructive ones. This process empowers people to manage problems in a practical way, improving emotional well-being and coping skills.
Commonly applied to anxiety, depression, and stress-related conditions, CBT is goal-oriented and time-limited. It combines cognitive strategies with behavioural techniques, making it an effective and evidence-based approach for many mental health issues.
- Persistent negative thoughts
- Excessive worry or anxiety
- Low mood or depression
- Difficulty concentrating
- Avoidance behaviours
- Irritability or restlessness
- Sleep disturbances
- Physical tension or discomfort
What are the underlying scientific principles?
Cognitive Model
Behavioural Activation
Empirical Testing
CBT uses evidence-based techniques. Clients test beliefs through behavioural experiments and reality checks, fostering critical thinking and validating rational alternatives to maladaptive cognitive patterns.
Empirical Testing
CBT uses evidence-based techniques. Clients test beliefs through behavioural experiments and reality checks, fostering critical thinking and validating rational alternatives to maladaptive cognitive patterns.
Collaborative Approach
Time-Limited Structure
CBT is goal-oriented and structured within a defined timeframe, focusing on measurable outcomes and practical strategies for sustainable psychological improvement.
How does it work?
Cognitive Behaviour Therapy (CBT) is a structured, evidence-based psychological approach that focuses on the connection between thoughts, emotions, and behaviours. It helps individuals identify and challenge negative thinking patterns, replacing them with healthier, more constructive alternatives. CBT is widely used to treat anxiety, depression, stress, and other mental health conditions. The therapy is collaborative, goal-oriented, and practical, often involving homework exercises to reinforce learning. By promoting self-awareness and problem-solving skills, CBT empowers individuals to manage challenges effectively and improve overall well-being. Its adaptability makes it suitable for diverse issues, offering long-term benefits beyond symptom relief.
Thought-Behaviour Link
CBT emphasises how thoughts influence emotions and behaviours. By recognising distorted thinking, individuals can change responses, reducing distress and fostering healthier coping strategies for everyday challenges.
Goal-Oriented Approach
Therapy sessions focus on specific, measurable goals. This structured method ensures progress tracking and empowers individuals to actively participate in their mental health improvement journey.
Evidence-Based Techniques
CBT uses scientifically validated strategies like cognitive restructuring and behavioural activation. These techniques help individuals challenge irrational beliefs and adopt practical solutions for emotional regulation.
Homework and Practice
Clients often complete exercises between sessions, such as journaling or exposure tasks. These reinforce learning, encourage self-reflection, and build resilience outside the therapy setting.
Short-Term Yet Effective
CBT is typically time-limited, often lasting 6–20 sessions. Despite its brevity, it delivers lasting benefits by equipping individuals with lifelong skills for managing thoughts and behaviours.
Wide Applicability
CBT treats anxiety, depression, phobias, and stress, and supports lifestyle changes. Its adaptability makes it effective across age groups and cultural contexts, enhancing accessibility and relevance.
When Is It Used?
Cognitive Behavioural Therapy (CBT) is a widely recognised, evidence-based approach for addressing mental health challenges. It is commonly used to treat conditions such as depression, anxiety disorders, post-traumatic stress disorder (PTSD), obsessive-compulsive disorder (OCD), and phobias. CBT is also effective for managing stress, insomnia, chronic pain, and coping with grief or trauma. By focusing on the link between thoughts, emotions, and behaviours, CBT helps individuals identify and change unhelpful patterns, fostering healthier coping strategies. Its structured, goal-oriented nature makes it suitable for both short-term interventions and long-term resilience building, often combined with medication or other therapies for optimal results.
Conditions and Issues Where CBT Is Commonly Applied
What are the therapy options that Transformations Clinical Psychology can offer me?
Please contact us or follow this link if you would like to set up an assessment with a psychologist at Transformations Clinical Psychologist.
Meet Our Team
Meet our friendly and experienced team, here to help you with confidence and care.








Amy Wang
Mandarin
English


We are here to support you
Please contact us or click on this link if you would like to see one of our experienced psychologists
FAQ
Q1. What happens in the first session? Do I need to prepare?
Your first appointment is 50–60 minutes. We’ll get to know you—what’s been hard, what you’d like to change, and what’s helped before. You’re welcome to bring notes or just come as you are; we’ll go at your pace. Please complete the online intake and consent forms beforehand. Sessions are available in person (Sydney) or via secure telehealth across Australia. We’ll finish with a clear plan and time for your questions. If you’re in immediate danger, call 000.
Q2. How do fees and Medicare/private insurance work? Do I need a GP referral?
You can book without a referral. If your GP provides a Mental Health Treatment Plan, you may be eligible for a Medicare rebate. We’ll check your eligibility and confirm your out-of-pocket cost before you commit. Private health (Extras) can’t be claimed with Medicare for the same session—please check your fund for coverage. If cost is a concern, let us know and we’ll talk through options.
Q3. Will my information be kept confidential?
Yes. Your sessions and records are kept private under strict legal and ethical standards. There are a few exceptions—if there’s a serious risk of harm, concerns about a child or vulnerable person, or a court order. If we ever need to share information, we’ll explain why, what will be shared, and involve you as much as possible.
